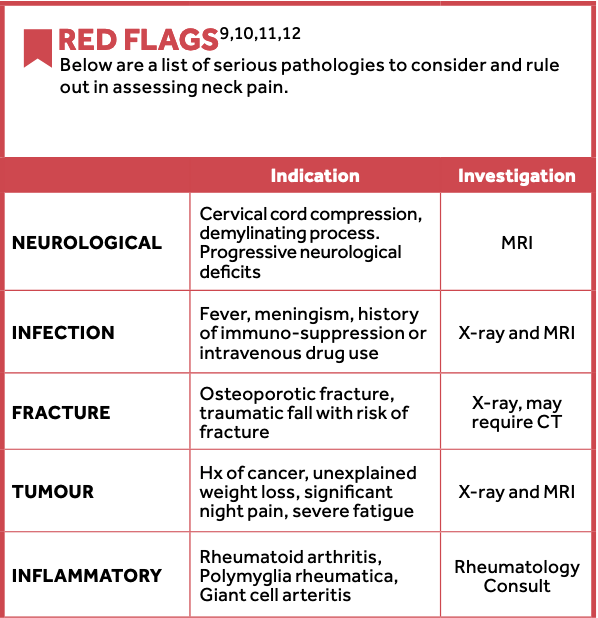
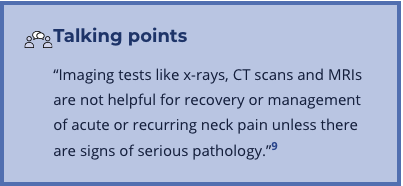
If NO Red Flags, continue with CORE Neck Tool Cardiovascular pathology (carotid arterial dissection, concurrent chest pain, myocardial ischemia) can present with neck and shoulder pain.
This is a focused examination for clinical decision-making in primary care. This tool guides primary care providers to recognize common mechanical neck pain and screen for other conditions where management may include investigations, exercise referrals and specific medications. Mechanical neck pain can present with neck, shoulder and/or arm pain. If your patient has an accompanying headache, it is recommended that you treat the headache symptoms first using the Headache Navigator.
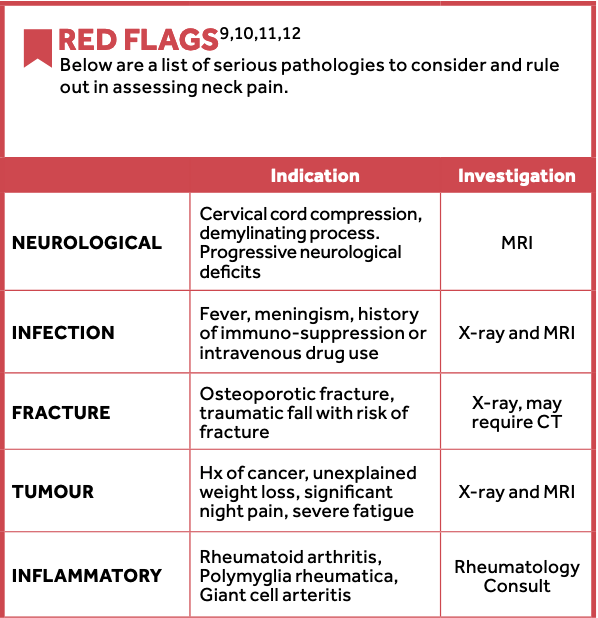
If NO Red Flags, continue with CORE Neck Tool Cardiovascular pathology (carotid arterial dissection, concurrent chest pain, myocardial ischemia) can present with neck and shoulder pain.
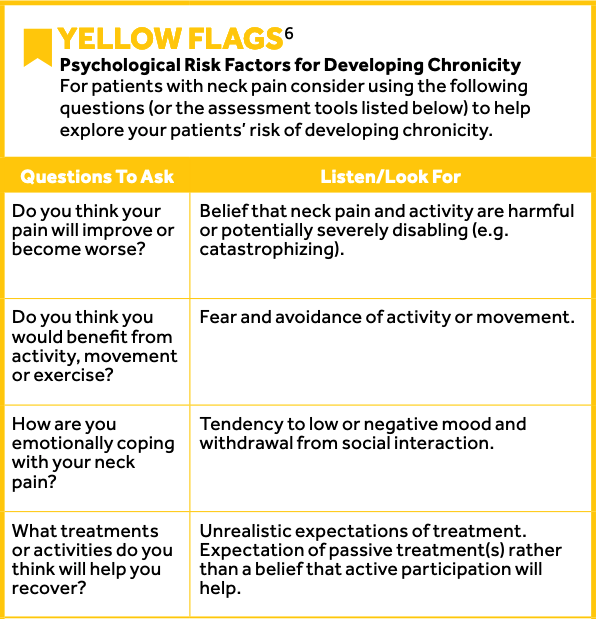
If NO Yellow Flags, continue with CORE Neck Tool
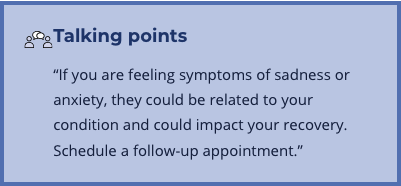
A patient with positive Yellow Flag(s) may benefit from education, support and targeted therapies to reduce risk of chronicity and could be screened for psychological conditions (e.g. anxiety, depression). Consider the following resources to support assessment and management of risk factors for chronicity; The Patient Health Questionnaire for Depression and Anxiety (PHQ-4)7; Pain Self Efficacy Questionnaire (PSEQ).8
The Headache Navigator assists primary care providers in managing primary headache disorders. It is based on the guideline and quick reference algorithm for the Primary Care Management of Headache in Adults produced by Towards Optimized Practice (TOP).
This is an examination which supports or refutes the differential diagnosis while assessing the severity of symptoms for prognosis
and treatment planning. This examination should take 5 minutes of the clinical assessment. The examination has been developed for
primary care providers.
Observation
Palpation
Movement
Neurological
Radiculopathy
If there are no Red flags
“Your examination today does not demonstrate that there are any Red flags present to indicate serious pathology, but if your symptoms persist for >6 weeks, schedule a follow-up appointment.”
Recommended
Patient education and exercise should be included as part of active management and may be delivered solely within primary care office visit.
Treatment may include:
Recommended number of treatment sessions = 1-6
Not Recommended
There is inconclusive evidence for the following:
Chronic (>3 months)
Recommended
Multimodal therapy and/or goal directed therapy including:
Active Rehabilitation therapy may include:
Recommended number of treatment sessions = 6-12 sessions
Not Recommended
There is inconclusive evidence for the following:
Acute (<3 months)
Recommended
In addition to the above treatment regimes for neck dominant pain, patients with arm dominant pain may find additional relief with the following:
Not Recommended
There has been no proven effectiveness of the following:
Chronic (>3 months)
Recommended
In addition to the above treatment regimes for neck dominant pain, patients with arm dominant pain may find additional relief with the following:
Not Recommended
There has been no proven effectiveness of the following:
Acute (<3 months)
Recommended
Start with:
Add or replace with
Not Recommended
Routine use of opioids:
Inconclusive
Chronic (>3 months)
Recommended
Start with:
Add or replace with
Not Recommended
Routine use of opioids:
Inconclusive
Acute (<3 months)
Recommended
Start with:
Add or replace with
For severe radiculopathy consider methylpredinisolone or dexamethasone for 5-7 days.
Chronic (>3 months)
Recommended
Start with:
Add or replace with
Consider a referral to the pain management options listed in the table below, if the following criteria are met:
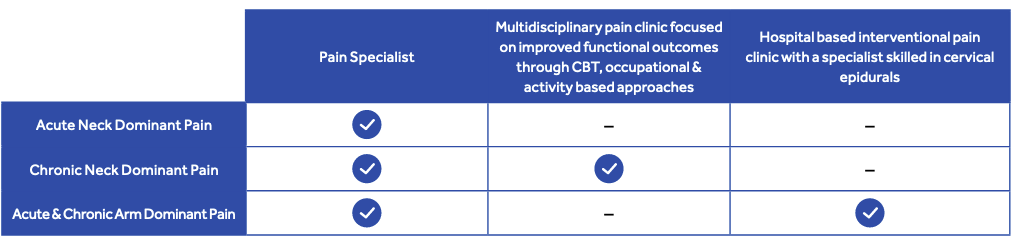
Pain management and referral
These recommendations are systematically developed statements to assist practictioner and patient decisions about appropriate health care for specific clinical circumstances. They should be used as an adjunct to sound clinical decision making. Refer to full guideline for migraine treatment in pregnancy.
Dosage may be increased every two weeks to avoid side effects. For most drugs, slowly increase to target dose
Abbreviations: hs – at bedtime; bid – twice a day; tid – three times a day
Adapted with permission from: Towards Optimized Practice. Guideline for primary care management of headache in adults. Edmonton, AB: Towards Optimized Practice. 2012 July. Available from: www.topalbertadoctors.org
These recommendations are systematically developed statements to assist practitioner and patient decisions about appropriate health care for specific clinical circumstances. They should be used as an adjunct to sound clinical decision making.
Adapted with permission from: Towards Optimized Practice. Guideline for primary care management of headache in adults. Edmonton, AB: Towards Optimized Practice. 2012 July. Available from: www.topalbertadoctors.org
These recommendations are systematically developed statements to assist practitioner and patient decisions about appropriate health care for specific clinical circumstances. They should be used as an adjunct to sound clinical decision making.
NOTE: If more than two attacks per day, consider transitional therapy while verapamil is built up (e.g. prednisone 60 mg for 5 days, then reduced by 10 mg every 2 days until discontinued)
Adapted with permission from: Towards Optimized Practice. Guideline for primary care management of headache in adults. Edmonton, AB: Towards Optimized Practice. 2012 July. Available from: www.topalbertadoctors.org



Kopjar B, Tetreault L, Kalsi-Ryan S, Fehlings M. Psychometric properties of the modified Japanese orthopaedic association scale in patients with cervical spondylotic myelopathy. Spine. 2014. 40(1): E23-28.
Hall H. Effective spine triage: Patterns of pain. Ochsner J. 2014 Spring; 14(1): 88-95.
Stiell IG, et al. The Canadian C-spine rule for radiography in alert and stable trauma patients. JAMA. 2001 Oct; 286(15):1841-8
Concussions Ontario [Internet]. 2015 [cited 2016 May 30]. Available from: http://concussionsontario.org/
British Columbia Ministry of Health, British Columbia Medical Association. Rheumatoid arthritis: diagnosis, management and monitoring [Internet]. 2012 Sep [cited 2016 Mar 8]. [Figure], Differentiate inflammatory from non-inflammatory arthritis; p. 2. Available from: http://www2.gov.bc.ca/gov/content/health/practitionerprofessional-resources/bc-guidelines/rheumatoid-arthritis
New Zealand Guidelines Group. New Zealand acute low back pain guide: Incorporating the guide to assessing psychosocial yellow flags in acute low back pain [Internet]. 2004 Oct [cited 2015 Nov 25]. Available from: http://www.acc.co.nz/PRD_EXT_CSMP/groups/external_communications/documents/guide/prd_ctrb112930.pdf
Kroenke K, Spitzer RL, Williams JBW, Lowe B. An ultra-brief screening scale for anxiety and depression: the PHQ-4. Psychosomatics [Internet]. 2009 Nov-Dec [cited 2015 Nov 20]; 50(6): 613-621. Available from: http://www.psychiatrictimes.com/all/editorial/psychiatrictimes/pdfs/scale-PHQ4.pdf
Nicholas MK. The pain self-efficacy questionnaire: Taking pain into account. Eur J Pain. 2007 Feb; 11(2): 153-63.
Cervical and thoracic spine disorders. In Hegmann KT, editor. Occupational medicine practice guidelines. Evaluation and management of common health problems and functional recovery in workers. 3rd ed. Elk Grove Village, IL: American College of Occupational and Environmental Medicine; 2011.
National Institute for Health and Clinical Excellence. Neck pain – non-specific. Clinical Knowledge Summaries. 2015 Apr.
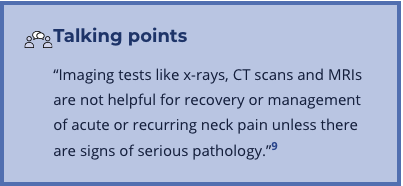
Canadian Association of Radiologists. Section D: Musculoskeletal system. Diagnostic Imaging Referral Guidelines. 2012. Available from: http://www.car.ca/en/standards-guidelines/guidelines.aspx
Canadian Association of Radiologists. Section J: Trauma. Diagnostic Imaging Referral Guidelines. 2012. Available from: http://www.car.ca/en/standards-guidelines/guidelines.aspx
Cook C, Hegedus E. Orthopedic physical examination tests: An evidence-based approach. Upper Saddle River, N.J.: Pearson Education, 2013.
Yung E, Asavasopon S, Godges JJ. Screening for head, neck, and shoulder pathology in patients with upper extremity signs and symptoms. J Hand Ther. 2010 Apr-Jun; 23(2): 173-85.
Wainner RS, et al. Reliability and diagnostic accuracy of the clinical examination and patient self-report measures for cervical radiculopathy. Spine. 2003 Jan 1; 28(1): 52-62.
Cote P, et al. Management of neck pain and associated disorders: A clinical practice guideline from the Ontario Protocol for Traffic Management (OPTIMa) Collaboration. Eur Spine J. 2016 Mar 16.
Rampersaud YR, Alleyne J, Hall H. Managing leg dominant pain. J Current Clinical Care. 2013 Jan; Educational Suppl.: 32-39.
National Institute for Health and Clinical Excellence. Neck pain – cervical radiculopathy. Clinical Knowledge Summaries. 2015 Apr.
National Opioid Use Guideline Group. Canadian guideline for safe and effective use of opioids for chronic non-cancer pain [Internet]. 2010 [cited 2016 May 30]. Available from: http://nationalpaincentre.mcmaster.ca/opioid/
Childs JD, et al. Neck pain: Clinical practice guidelines linked to the International Classification of Functioning, Disability, and Health from the Orthopaedic Section of the American Physical Therapy Association. 2008. J Orthop Sports Phys Ther. 38(9):A1-A34.
Hall H, Alleyne J, McIntosh G, Cote P. A pain in the neck. Journal of Current Clinical Care. 2015; 5(1):24-34.
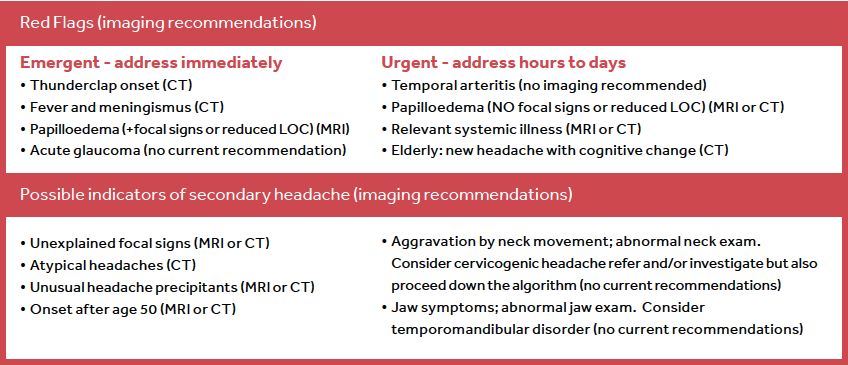
Headache Imaging Pathway. Developed as part of the Diagnostic Imaging Appropriateness (DI-APP) Tools in Primary Care project by University Health Network, Health Quality Ontario, Ministry of Health and Long-Term Care. 2015.
Toward Optimized Practice. Guideline for primary care management of headache in adults. Edmonton, AB: Toward Optimized Practice. 2012 July. Available from: www.topalbertadoctors.org
National Institute for Health and Clinical Excellence. Headaches: Diagnosis and management of headaches in young people and adults. Clinical guideline 150: Methods, evidence and recommendations. 2012 Sep.
Choosing Wisely Canada, Canadian Association of Radiologists. Imaging tests for headaches: When you need them – and when you don’t. 2014. Available from: http://www.choosingwiselycanada.org/
Canadian Association of Radiologists. Section A: Central nervous system. Diagnostic Imaging Referral Guidelines. 2012. Available from: http://www.car.ca/en/standards-guidelines/guidelines.aspx
This Tool was developed as part of the Knowledge Translation in Primary Care Initiative which is led by CEP with collaboration from Ontario College of Family Physicians and Nurse Practitioners’ Association of Ontario. Clinical leadership for the development of the tool was provided by Drs. Julia Alleyne MD, CAC(SEM), FCFP and Arun Radhakrishnan MSc, MD, CM CCFP and was subject to external review by primary care providers and other relevant stakeholders. This Tool was funded by the Government of Ontario as part of the Knowledge Translation in Primary Care Initiative.
This Tool was developed for licensed health care professionals in Ontario as a guide only and does not constitute medical or other professional advice. Primary care providers and other health care professionals are required to exercise their own clinical judgment in using this Tool. Neither the Centre for Effective Practice (“CEP”), Ontario College of Family Physicians, Nurse Practitioners’ Association of Ontario, Government of Ontario, nor any of their respective agents, appointees, directors, employees, contractors, members or volunteers: (i) are providing medical, diagnostic or treatment services through this Tool; (ii) to the extent permitted by applicable law, accept any responsibility for the use or misuse of this Tool by an individual including, but not limited to, primary care providers or entity, including for any loss, damage or injury (including death) arising for or in connection with the use of this Tool, in whole or in part; or (iii) give or make any representation, warranty or endorsement of any external sources referenced in this Tool (whether specifically named or not) that are owned or operated by third parties, including any information or advice contained therein.
CORE Neck Tool and Headache Navigator is a product of the Centre for Effective Practice. Permission to use, copy, and distribute this material for all non-commercial and research purposes is granted, provided the above disclaimer, this paragraph and the following paragraphs, and appropriate citations appear on all copies, modifications, and distributions. Use of CORE Neck Tool and Headache Navigator for commercial purposes or any modification of the tool are subject to charge and use must be negotiated with Centre for Effective Practice (Email: info@effectivepractice.org).
For statistical and bibliographic purposes, please notify the Centre for Effective Practice (info@effectivepractice.org) of any use or reprinting of the tool. Please use the below citation when referencing the tool: Reprinted with Permission from Centre for Effective Practice (Summer 2016). CORE Neck Tool and Headache Navigator. Toronto. Centre for Effective Practice.
Developed by
In collaboration with