Note: Updates to the Notification of the Corner section in the HTML tool have not been reflected in the pdf tool.
Track One: Natural death is reasonably foreseeable
Note: Updates to the Notification of the Corner section in the HTML tool have not been reflected in the pdf tool.
There are tooltips Tooltip content throughout this tool that you can place your cursor over to view the definition of certain terms. For the full list of definitions, see Definition of terms.
On March 17, 2021, changes to the MAID legislation came into force through Bill C-7.1 These changes allow MAID for eligible persons who wish to pursue a medically assisted death, whether their natural death is reasonably foreseeable (Track One) or not reasonably foreseeable (Track Two).2
This resource highlights key considerations and recommends processes for the provision of MAID by Clinician For this resource, the term Clinician refers to the medical or nurse practitioner that is overseeing the provision of MAID for an individual patient. This role may include, but is not limited to, receiving a patient request for MAID, conducting the first eligibility assessment, and administering or prescribing the drug protocol for the provision of MAID. It is recommended that this Clinician be responsible for ensuring that all relevant documentation is obtained and included in the patient’s medical record. In instances where the Clinician responsible for the provision of MAID is not the Most Responsible Provider (MRP) (e.g. in cases of conscientious objection and patient referral), the MRP will remain involved to direct the coordination of care for the patient (excluding the provision of MAID). For this resource, the term Second Clinician refers to the medical or nurse practitioner that conducts the second, independent eligibility assessment of the patient. This role may also include administering or prescribing the drug protocol for the provision of MAID.
*The MRP and the Clinician OR Second Clinician may have overlapping roles and responsibilities or may be the same individual.. It is based on extensive consultations with key stakeholder organizations and regulatory bodies, and it is intended to explain, not circumvent, existing legal requirements, regulatory body requirements or institutional processes that have been established.
While this resource is based on the best available information, there may be gaps in the process that cannot be addressed at this time. Every effort will be made to incorporate updates as new information becomes available.
The revised law creates a two-track approach to procedural safeguards for Clinicians to follow, based on whether or not a person’s natural death is reasonably foreseeable.2
The recent legislative changes have not altered the meaning of “reasonably foreseeable natural death.” Clinicians can continue to rely on the guidance previously provided by the court and the clinical community to inform their assessment of whether a patient’s natural death is reasonably foreseeable or not, and therefore, which procedural safeguards apply.3
For more information about Track One, see the CEP’s resource on Medical Assistance in Dying (MAID) in Ontario Track One: Natural Death is Reasonably Foreseeable.4
Additional safeguards apply for patients whose natural death is NOT reasonably foreseeable. For example, this includes requiring that patients undergo a 90-day assessment period before receiving MAID.2,3
Continue with this tool for Track Two: Track Two: Natural death is NOT reasonably foreseeable
Bill 84, the Medical Assistance in Dying Statute Law Amendment Act, 2017, amended six existing Ontario statutes.5 Notably, Bill 84 included an amendment to the Coroners Act to ensure effective oversight of MAID.
These records should be on-hand and accessible to support an efficient and effective investigation by the Office of the Chief Coroner. Note: The use of Clinician Aid A, B, and C is voluntary and is used in this Resource as an option for documenting MAID requests and assessing eligibility.
A patient’s inquiry about MAID can take many forms:7
Clinicians with conscientious objections must respectfully and non-judgementally inform their patients that they will not assess or provide MAID and refer patients to another medical or nurse practitioner, institution or agency that is willing to facilitate the provision of MAID, such as the Ministry’s CCS The CCS supports patients, family members/ caregivers acting on patients’ behalves and Clinicians by providing information about end-of-life options, including MAID, and by helping to connect with MAID services.
Patients and family members/caregivers acting on their behalves may access the CCS to request being connected to a Clinician who will provide MAID services, including eligibility assessments.
For Clinicians who are unwilling or unable to provide MAID, the CCS can help to connect their patients to Clinicians who are willing to provide MAID services.
The CCS will also support patient access to MAID by helping Clinicians connect with a:
• Clinician who can provide the second assessment needed to confirm that a patient meets all eligibility criteria, as required by the federal MAID legislation;
• Community pharmacist who will dispense the drugs required for MAID; and
• Clinician who will prescribe or administer the drugs required for MAID, if needed. . The referral must be made promptly to ensure that patients are not exposed to unnecessary delays or adverse clinical outcomes (e.g. a decline in capacity). Irrespective of a patient’s desire to explore MAID through another nonobjecting Clinician, institution or agency (e.g. CCS), Clinicians must continue to provide ongoing care (excluding the provision of MAID) to the patient.3,8,9
Clinicians must follow the requirements, policies and guidelines set out by their respective regulatory colleges regarding conscientious objection and patient referral. Clinicians must adhere to additional directives outlined by their institution or agency (e.g. institutions may implement specific processes and policies to facilitate patient referral and to ensure access to care).
Clinicians who choose not to assess or provide MAID can either make a referral through their professional networks or the Ministry’s CCS.



INFO: the Ministry has created the CCS to support referrals by Clinicians, patients and family members/caregivers acting on their behalves. The CCS information line (1-866-286-4023) is available 24/7. Referral services are available Monday – Friday, 9 am – 5 pm ET, with voicemail available after hours. Both the information line and referral services are available in English and French (translation for other languages can be requested), and TTY is available at 1-844-953-3350.
Patients must submit a formal written request for MAID, signed and dated in the presence of one independent‡ witness (e.g. Clinician Aid A).10 The formal written request can only be signed and dated by the patient after they have been informed by a Clinician that they have a grievous and irremediable medical condition.
‡To meet the legal conditions for independent witness, the following criteria must be met:1
*These individuals would also be excluded from acting as a witness if they are a beneficiary of the person’s will or if they would receive a financial benefit from the person’s death.11
Additional considerations:
An express desire to end one’s life through MAID requires a careful exploration to understand the patient’s suffering, as well as inducements that may arise from psychosocial or non-medical conditions and circumstances. If psychosocial factors (e.g. grief, loneliness, stigma, shame) or lack of resources (e.g. barriers to accessing medical care, assistive devices, psychological supports) motivates the patient’s request, then efforts should be made to alleviate these concerns.
This is an opportunity for the Clinician to:
Patients are not required to undergo any procedure or treatment that is not acceptable to them.
Federal MAID legislation:1
The federal reporting requirements capture MAID deaths and written requests for MAID, even if a MAID death never occurs (e.g. if the patient dies beforehand, if they were deemed ineligible, if they change their mind).
A patient’s written request for MAID may take any form, including a text message or an email. The patient does not have to provide a formal written request (i.e. signed, dated, and witnessed) for it to be reported. As long as it is an explicit request for MAID, regardless of written format, Clinicians are to report this. The Most Responsible Provider For this resource, the term Clinician refers to the medical or nurse practitioner that is overseeing the provision of MAID for an individual patient. This role may include, but is not limited to, receiving a patient request for MAID, conducting the first eligibility assessment, and administering or prescribing the drug protocol for the provision of MAID. It is recommended that this Clinician be responsible for ensuring that all relevant documentation is obtained and included in the patient’s medical record. In instances where the Clinician responsible for the provision of MAID is not the Most Responsible Provider (MRP) (e.g. in cases of conscientious objection and patient referral), the MRP will remain involved to direct the coordination of care for the patient (excluding the provision of MAID). For this resource, the term Second Clinician refers to the medical or nurse practitioner that conducts the second, independent eligibility assessment of the patient. This role may also include administering or prescribing the drug protocol for the provision of MAID.
*The MRP and the Clinician OR Second Clinician may have overlapping roles and responsibilities or may be the same individual. would report a patient’s written request for MAID. If there is no MRP identified with respect to the receipt of a written request, the Clinicians involved (or the CCS or administrative body, where applicable) must determine which Clinician will be responsible for reporting. Note: Neither the federal legislation nor the Regulations allow for delegation of reporting on MAID to other individuals or administrative staff.12 It is also possible for multiple Clinicians to receive a written request for MAID from a patient and be unaware that the same patient requested MAID from other Clinicians. In this scenario, each Clinician is required to report. The Canadian MAID Data Collection Portal will be able to discern multiple independent reports related to one patient through common data points that are reported (i.e. date of birth and health card number).13
Ontario has taken on a hybrid approach to federal reporting, in that:
Clinicians will report to Health Canada via the Canadian MAID Data Collection Portal in the following situations when a written request for MAID has been received:
Note:
INFO: the Ministry has created Clinician Aids to record the patient’s request and the results of the eligibility assessments:
The requirements for capacity to undergo MAID are the same as the requirements for any health care treatment. The use of existing procedures for capacity assessments are encouraged.14
Two-part question to assess capacity:15

A patient’s request for MAID must be voluntary and not result from external pressure.1,8,14
Reasonable measures should be taken to assess if the patient’s decision has been made freely, without coercion or undue influence from family members/caregivers, health care providers or others.
A patient must provide informed consent to receive MAID, after being informed of alternate care options available to alleviate suffering, including access to devices, specialists and palliative care.1
For consent to be informed, a patient must understand the six components of informed consent, as outlined in the Health Care Consent Act, 1996:15
The patient must understand that consent can be withdrawn at any time before undergoing MAID, without negative consequences on the Clinician-patient relationship or the care provided to the patient.
The Clinician must take reasonable steps to ensure that a patient understands the information provided about their health status and MAID. If a patient has difficulty communicating, the Clinician must take necessary measures to provide a reliable means for the patient to understand the information provided and communicate their decision.1,8,14
Clinicians should consider the following to determine if their patient meets the criteria for informed consent.
The patient:
*A total of 52 cases have proceeded to full or external post-mortem examination since the legalization of MAID in 2016. Of the 52 cases, 45 occurred in 2016, before Ontario’s Medical Assistance in Dying Statute Law Amendment Act, 2017 came into force and amended the Coroners Act, R.S.O. 1990, c. C.37. As of 2017, all MAID cases are reviewed by the Office of the Chief Coroner (OCC) but do not necessarily meet the criteria for investigation under the amended Coroners Act, R.S.O. 1990, c. C.37, resulting in few post-mortem examinations. Since the amendments, there have been a total of 7 post-mortem examinations from 2017-2021.16

A patient’s condition is grievous and irremediable if ALL of the following criteria are met:17

The following are Track Two procedural safeguards from the law:
Two independent* Clinicians (e.g. two medical practitioners, two NPs, or one medical practitioner and one NP) must separately conduct an assessment to ensure that a patient meets ALL criteria required to be eligible for MAID and provide their opinion in writing to confirm a patient’s eligibility.1,8,9,14
*To meet the legal conditions for independence, each Clinician must ensure that they:1
If neither of the clinicians have expertise in the condition that is causing the person’s suffering, the clinician providing MAID must consult with a medical practitioner or nurse practitioner with that expertise and must share the results of that consultation with the practitioner providing the written opinion confirming the patient is eligible for MAID.
It is not necessary to have a specialty designation or certification to have expertise. Expertise could be obtained through education, training or experience (e.g., treating patients with a similar condition).
For patients whose natural death is NOT reasonably foreseeable, it is required that a minimum of 90-days be taken for the assessment of the patient’s eligibility. This period can be shortened by the Clinician providing MAID if both Clinicians are of the opinion that the loss of the patient’s capacity to provide consent to receive MAID is imminent and if both assessments have been completed.1 This assessment will ensure that enough time is devoted to exploring all relevant aspects of the patient’s situation, including whether some treatments or services could help to reduce their suffering, such as counselling services, mental health and disability support services, community services and palliative care.
The 90-day period begins on the day of the patient’s first MAID eligibility criteria assessment (e.g. the day on which the Clinician first considers or reflects on information that forms part of a MAID assessment, such as reviewing the patient’s file or meeting with the patient).

There is no formal notification process to inform family members/caregivers of a patient’s decision to pursue MAID. Clinicians can ask their patient if they would like their family members/caregivers involved. However, the patient is not obligated to inform their family members/caregivers of their decision to pursue MAID. With the patient’s consent, discussions between the Clinician and family members/caregivers can occur either before or after a formal request for MAID has been made. It is also important to note that family members/caregivers cannot override the patient’s request for MAID.
To provide MAID may require a collaborative care team, including allied health care providers, support care personnel and administrators, depending on the clinical practice setting. Early in the process, Clinicians are encouraged to identify and engage the appropriate individuals and to discuss the roles and responsibilities of each team member in the provision of MAID (e.g. pharmacist).
It is encouraged that a care team review and debrief after MAID has been provided to a patient. The process can be an overwhelming and emotional experience for the Clinician and care team. The use of wellness resources and supports is encouraged to promote self-care.

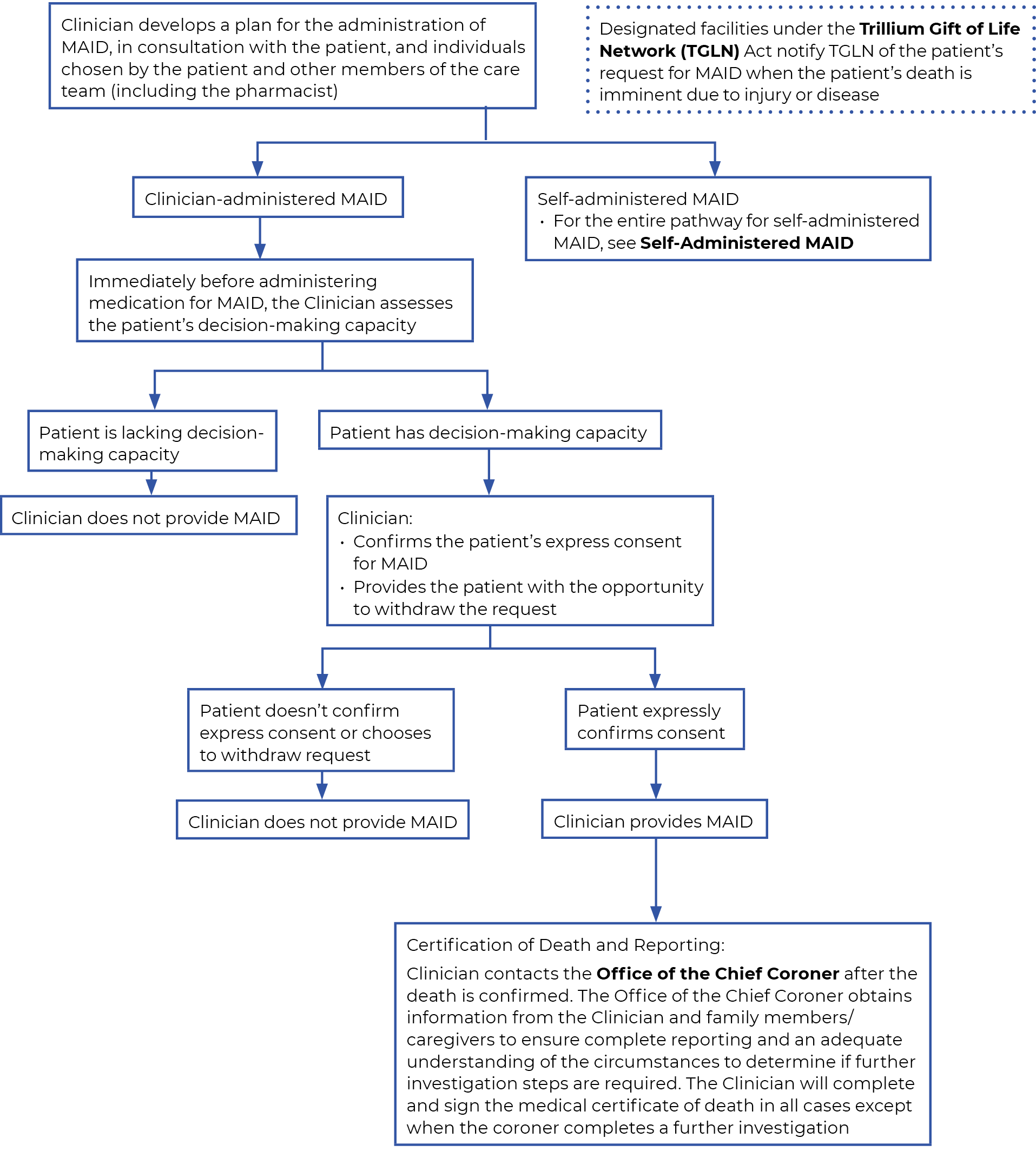
The Clinician develops a care plan for the provision of MAID through discussions with the patient, individuals chosen by the patient and other care team members.

Trillium Gift of Life Network (TGLN)
Patients may be eligible to donate tissue and organs after MAID. Offering the opportunity for donation is part of providing high-quality end-of-life care. Through collaboration with the Clinician and TGLN, this conversation should occur early enough for patients to include their decision to donate into their plans for MAID.

Designated facilities and sites are required to notify TGLN of all patients whose death is imminent due to injury or disease as per section 8.1 of the TGLN Act.20
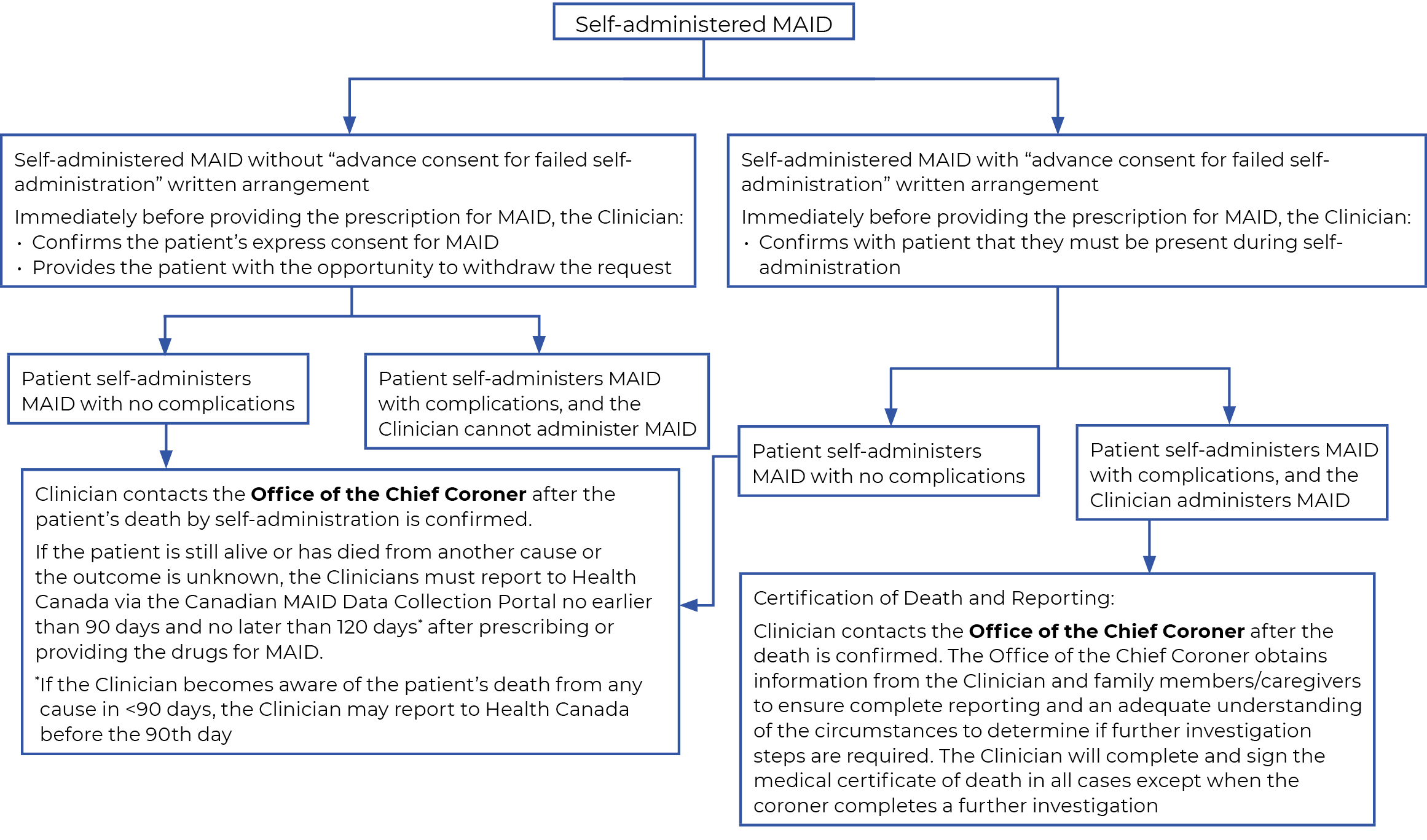
Patients who choose to self-administer MAID may enter into written arrangements allowing for Clinician-administered MAID if complications follow self-administration. Clinicians may administer MAID to a patient who loses the capacity to consent after
self-administering if:3
The Clinician who prescribes or obtains a substance to provide MAID must inform the pharmacist that the substance is intended for MAID, before a pharmacist dispenses the substance.
It is encouraged that pharmacists are engaged as early as possible, once the Clinician is aware that the patient is eligible for MAID.9
Collaboration at an early stage will ensure that eligible patients can access the required medications and supplies promptly.
Discussions with the pharmacist should include:9
Within 30 days of dispensing the drugs, the dispensing pharmacist is required to report to Health Canada via the Canadian MAID Data Collection Portal.
Clinicians must exercise their clinical judgment to determine the appropriate drug protocol to follow for the provision of MAID.
Irrespective of the chosen drug protocol for MAID, Clinicians should ensure that the patient is comfortable and that pain and anxiety are controlled. The cost of drugs, including the backup kit, for all eligible patients is covered regardless of the mode of administration.
Under the current law, all Clinician-administered and self-administered MAID deaths must be reported to the Office of the Chief Coroner. Notification is now conducted electronically using the Mandatory Death Reporting (MDR) form. The MDR form must be submitted by the end of the next business day following the MAID death.22 Once a death is reported, the Office of the Chief Coroner will speak with Clinicians and family members/caregivers. Clinicians must be prepared to provide the required information to make the process as efficient, effective and appropriate as possible.
It is recommended that Clinicians who provide MAID have complete medical records on-hand and accessible to share information that the Coroner needs for complete reporting and to determine if further investigation of the death is required. The Clinician will complete and sign the death certificate in all cases except for occasions when the coroner completes further investigation.
A physician who is licensed to practice medicine in Ontario.
A registered nurse who is licensed to practice as a nurse practitioner in Ontario.
For this resource, the term Clinician refers to the medical or nurse practitioner that is overseeing the provision of MAID for an individual patient. This role may include, but is not limited to, receiving a patient request for MAID, conducting the first eligibility assessment, and administering or prescribing the drug protocol for the provision of MAID. It is recommended that this Clinician be responsible for ensuring that all relevant documentation is obtained and included in the patient’s medical record. In instances where the Clinician responsible for the provision of MAID is not the Most Responsible Provider (MRP) (e.g. in cases of conscientious objection and patient referral), the MRP will remain involved to direct the coordination of care for the patient (excluding the provision of MAID). For this resource, the term Second Clinician refers to the medical or nurse practitioner that conducts the second, independent eligibility assessment of the patient. This role may also include administering or prescribing the drug protocol for the provision of MAID.
For patients whose natural death is NOT reasonably foreseeable, it is required that one of the two Clinicians (who confirm the patient’s eligibility for MAID) has expertise in the condition causing the patient’s suffering or that a Clinician is consulted who has such expertise.3 The federal government has clarified that the expertise must be in the condition that is causing the patient the greatest suffering.3 See Consulting Clinician with “expertise” in the patient’s condition for more information.
The CCS supports patients, family members/ caregivers acting on patients’ behalves and Clinicians by providing information about end-of-life options, including MAID, and by helping to connect with MAID services.
The care coordination service information line is available 24 hours a day, 7 days a week and may be reached toll free at 1-866-286-4023.
Patients who choose to self-administer MAID may enter into written arrangements allowing for Clinician-administered MAID if that self-administration of MAID fails.3 This applies to either Track One or Track Two. Clinicians may administer MAID to a patient who loses the capacity to consent after self-administering if the patient meets the criteria outlined in “Advance Consent for Failed Self-Administration.”3
*The MRP and the Clinician OR Second Clinician may have overlapping roles and responsibilities or may be the same individual.



An Act to amend the Criminal Code (medical assistance in dying) (Bill C-7), 2nd Sess, 43rd Leg, Canada, 2021 (assented to March 17, 2021).
Government of Canada Department of Justice. Canada’s new medical assistance in dying (MAID) law. 2021. [cited 2021 April 5]. Available from: https://www.justice.gc.ca/eng/cj-jp/ad-am/bk-di.html
College of Physicians and Surgeons of Ontario. Advice to the Profession: Medical Assistance in Dying. 2021. [cited 2021 April 20]. Available from: https://www.cpso.on.ca/Physicians/Policies-Guidance/Policies/Medical-Assistance-in-Dying/Advice-to-the-Profession-Medical-Assistance-in-Dyi#:~:text=This%20criminal%20prohibition%20applied%20to,the%20request%20of%20the%20patient.
Centre for Effective Practice. Medical Assistance in Dying (MAID) in Ontario: Track Two. 2021. [cited 2021 April 10]. Available from:
Bill 84: An Act to amend various Acts with respect to medical assistance in dying (ON). 2017. [cited 2017 November 2]. Available from: https://www.ontario.ca/laws/statute/s17007
Centre for Effective Practice. MAID. 2021. [cited 2021 April 10]. Available from:
Branigan M. Desire for hastened death: exploring the emotions and the ethics. 2015. [cited 2016 September 30]. Curr Opin Support Palliat Care. 9(1):64-71.
College of Nurses of Ontario: Guidance on Nurses’ Roles in Medical Assistance in Dying. 2021. [cited 2016 June 27]. Available from: https://www.cno.org/globalassets/docs/prac/41056-guidance-on-nurses-roles-in-maid.pdf
Ontario College of Pharmacists: Medical Assistance in Dying – Guidance to Pharmacists and Pharmacy Technicians. 2021. [cited 2021 April 30]. Available from: http://www.ocpinfo.com/library/practice-related/download/PhysicianAssistedDeath.pdf
Ontario Central Forms Repository. Clinician Aid A – Patient Request for Medical Assistance in Dying. 2021. [cited 2021 May 3]. Available from: http://www.forms.ssb.gov.on.ca/mbs/ssb/forms/ssbforms.nsf/FormDetail?OpenForm&ACT=RDR&TAB=PROFILE&SRCH=1&ENV=WWE&TIT=3889&NO=014-3889-22E
Government of Canada Department of Justice. Legislative Background: Bill C-7: Government of Canada’s Legislative Response to the Superior Court of Québec Truchon Decision – Part III – Safeguards for MAID. 2021. [cited 2021 April 10]. Available from: https://www.justice.gc.ca/eng/csj-sjc/pl/ad-am/c7/p4.html
Government of Canada. Guidance for reporting on medical assistance in dying. 2021. [cited 2021 June 15]. Available from: https://www.canada.ca/en/health-canada/services/medical-assistance-dying/guidance-reporting-summary/document.html#2.0
Health Canada Expert.
College of Physicians and Surgeons of Ontario Policy Statement #4-16: Medical Assistance in Dying. 2016. [cited 2016 June].
Health Care Consent Act, 1996, S.O. 1996, c. 2, Sched. A
Ontario Ministry of Health Expert.
Government of Canada. Grievous and irremediable medical condition. 2021. [cited 2021 April 10]. Available from: https://www.canada.ca/en/health-canada/services/medical-assistance-dying.html#grievous
Health Canada. (2021). Areas of Inquiry about Bill C-7 Implementation.
Downie J. MAiD in Canada 2021 From C-14 to C-7. [PowerPoint presentation]. 2021. [cited 2021 April 10].
Trillium Gift of Life Network Act, R.S.O. 1990.
Criminal Code, R.S.C., 1985, c. C-46, s. 241.2 (3.5).
Ministry of the Solicitor General, Office of the Chief Coroner. Checklist for MAID Providers [Internet]. 2023. Available from: https://files.ontario.ca/moh-maid-process-overview-checklist-en-2023-08-14.pdf
This Resource was developed as part of the Knowledge Translation in Primary Care Initiative, led by CEP with collaboration from OCFP and NPAO. Clinical leadership for the development of the resource was provided by Dr. Sandy Buchman, MD CCFP (PC) FCFP, with Dr. Jocelyn Downie, CM, FRSC, FCAHS, SJD, providing feedback on the legal content for the 2021 update. The resource was subject to external review by health care providers and other relevant stakeholders. This resource was funded by the Government of Ontario as part of the Knowledge Translation in Primary Care Initiative.
This Resource was developed for licensed health care professionals in Ontario as a guide only and does not constitute medical or other professional advice. Health care professionals are required to exercise their own clinical judgment in using this Resource. Neither the Centre for Effective Practice (“CEP”), Ontario College of Family Physicians, Nurse Practitioners’ Association of Ontario, Government of Ontario, nor any of their respective agents, appointees, directors, officers, employees, contractors, members or volunteers: (i) are providing medical, diagnostic or treatment services through this Resource; (ii) to the extent permitted by applicable law, accept any responsibility for the use or misuse of this Resource by any individual including, but not limited to, primary care providers or entity, including for any loss, damage or injury (including death) arising from or in connection with the use of this Resource, in whole or in part; or (iii) give or make any representation, warranty or endorsement of any external sources referenced in this Resource (whether specifically named or not) that are owned or operated by third parties, including any information or advice contained therein.
Medical Assistance in Dying (MAID) in Ontario Track Two: Natural Death is NOT Reasonably Foreseeable is a product of the Centre for Effective Practice. Permission to use, copy, and distribute this material for all non-commercial and research purposes is granted, provided the above disclaimer, this paragraph and the following paragraphs, and appropriate citations appear in all copies, modifications, and distributions. Use of the Medical Assistance in Dying (MAID) in Ontario Track Two: Natural Death is NOT Reasonably Foreseeable Resource for commercial purposes or any modifications of the resource are subject to charge and use must be negotiated with the Centre for Effective Practice (Email: info@cep.health).
For statistical and bibliographic purposes, please notify the Centre for Effective Practice (info@cep.health) of any use or reprinting of the resource. Please use the below citation when referencing the Resource: Reprinted with Permission from Centre for Effective Practice. (Revised September 2021). Medical Assistance in Dying (MAID) in Ontario Track Two: Natural Death is NOT Reasonably Foreseeable. Toronto: Centre for Effective Practice.
Developed by
In collaboration with