The following resource has been developed to address the legalization of cannabis. The resource is designed to help primary care providers in discussing non-medical cannabis with their adult (19+) patients, including educating on the harms and benefits of cannabis as well as general harm reduction. This resource is not intended to address medical cannabis.
Non-Medical Cannabis Resource
It is important that providers provide a safe, non-judgmental environment to allow for open dialogue. Counsel patients that use non-medical cannabis on harm reduction techniques and potential risk factors. If you identify problematic use or behaviour, screen for Cannabis Use Disorder and/or cannabis related mental health issues.
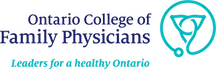
Screening for cannabis use New
Providers should screen all patients in their practice to ascertain their cannabis use. Patients who may have previously declined to inform their providers regarding their use may feel more comfortable disclosing cannabis use given legalization.
If you are concerned about potential problematic cannabis use, consider screening using the Cannabis Use Disorder Identification Test (CUDIT) or Cannabis Abuse Screening Test (CAST).1,2
For more general screening to determine whether patients may be using other substances problematically, consider the CAGE Adapted to Include Drugs for adults or the Brief Screener for Alcohol, Tobacco, and other Drugs or the CRAFFT Screening Tool for Adolescent Substance Abuse for youth.3,4
Therapeutic intent
Patients may be using non-medical cannabis with therapeutic intent for conditions including chronic pain, arthritis, or anxiety. In most cases there is insufficient evidence to recommend the use of cannabis for these conditions. Ensure first- and second-line pharmacological and non-pharmacological management of patients’ other health conditions is trialled prior to discussions about medical or non-medical cannabis.
Benefits/harms for patients using cannabis New
Ensure all patients, especially those considering new cannabis use, are aware of the potential risks prior to use.
Benefits & harms of cannabis use
Benefits
Medically indicated as a potential third-line treatment for:
- Refractory neuropathic or palliative pain
- Chemotherapy induced nausea and vomiting
- Spasticity in multiple sclerosis and spinal cord injury
- Patients with these conditions may have reduced pain and symptom improvement (i.e. nausea and vomiting or spasticity).
- Little evidence is available about the benefits for
other conditions commonly cited for therapeutic non-medical use.
Harms*
Patients using cannabis may experience:
- Cognitive issues (e.g. impaired memory) NNH = 12
- Disorientation or confusion NNH = 15
- Central nervous system effects NNH = 4
- Dizziness NNH = 5
- Speech disorders NNH = 5
- Numbness NNH = 4
- Ataxia or muscle twitching NNH = 6
- Some patients may experience serious psychiatric issues, including dissociation or acute psychosis. NNH = 20
*Given previous exposure and difficulty in conducting a true placebo control trial, it is thought that the harms may be underestimated in these findings.
Talking point
Benefits & harms of cannabis use
- “Smoking cannabis, like tobacco smoking, can have long-terms risks to your health including respiratory, reproductive, or memory issues.”
- “There is no good evidence to show cannabis is effective for most conditions. If you are using cannabis for other health issues, let’s discuss them and make sure we are managing them well with with treatments that have more evidence.”
- “While many people use cannabis to reduce their anxiety, it may in some cases make anxiety worse.”
- “Using cannabis may make you feel more relaxed and you may feel your anxiety is reduced. This is only a short-term fix; as the cannabis wears off you may actually feel an
increase in anxiety.”
Advising special populations
For patients with specific health risk factors or comorbidities, cannabis use may increase adverse health events. Advise patients with specific health concerns accordingly:
Mental health5
If your patient or an immediate family member has a history of psychosis, their risk of cannabis-related psychosis is increased. Cannabis use may exacerbate or trigger underlying mental health issues.
Older adults
Older adults may have age-related changes that could impact the outcome of their cannabis use, even if they have used cannabis previously. Evidence is limited in the older adult population, but age-related concerns may be a factor even for patients who have used cannabis previously.
Preconception and maternal health5
If your patient is pregnant, or is considering pregnancy, cannabis could harm their fetus or newborn. There is evidence that cannabis use may affect fertility in both men and women.
Use of cannabis during pregnancy increases risk of anemia.
Use of cannabis during pregnancy can lead to decreased birth weight, increased placement in neonatal care units, and child development and behavioural problems.
If your patient is breastfeeding, advise your patient that THC does pass into breastmilk and therefore to the baby but the impacts to the baby are unknown.
Cannabis use and driving
Cannabis use significantly increases risk of motor vehicle accidents – patients should wait at least 6-8 hours after using dry cannabis before driving or operating any heavy machinery and 8-12 hours if the patient ingests cannabis. This range may vary and is dependent on the amount and potency of the cannabis used, and the individual patient.
Ensure patients are aware of the current driving penalties in their province or territory if found under influence of cannabis.
Ensure patients are aware of the effects cannabis can have on driving: Canadian Centre on Substance Use and Addiction Drug Impaired Driving Toolkit
Cardiovascular
If your patient has previous cardiovascular events or cardiovascular risk factors, using dried and smoked cannabis could lead to elevated risk of stroke or adverse events.
Respiratory
Cannabis use, specifically dried and smoked cannabis, can exacerbate respiratory comorbidities and increase risk of additional respiratory concerns (e.g. chronic bronchitis, shortness of breath)
Substance use
If your patients or an immediate family member has a history of substance use disorder, additional harm reduction and precaution should be exercised.
Concurrent use of cannabis and other substances, including alcohol, results in increased impairment-related risks. Tobacco is considered more addictive than cannabis. Combining tobacco and cannabis can result in an increased risk of developing addiction to tobacco which can lead to regular use of cannabis.
Youth and younger adults
Population based studies have shown longer lasting cognitive effects including memory and attention problems in youth under the age of 25.
Ensure younger patients and their families are appropriately informed and supported: CAMH Cannabis Health Information & Resources
Harm reduction
Cannabis is addictive, though not everyone who uses it will develop an addiction. For any patients using cannabis, or considering using cannabis, ensure that appropriate harm reduction measures are communicated. Applying harm reduction principles can help to reduce the risk of adverse effects or problematic use.
For additional supports on harm reduction messages try the University of Victoria Take Care with Cannabis handout or CAMH’s Cannabis Lower Risk Guidelines.
Advise your patients to watch for symptoms of high cannabis toxicity, including:
- Auditory and visual hallucinations
- Paranoid delusions
- Confusion and amnesia
- Rapid breathing, high heart rate and elevated blood pressure
If these occur advise patients to call 911, local poison control centre, healthcare provider or the emergency department of your nearest hospital.
Talking point
Harm reduction measures to communicate to patients7,8
- “Try to defer use until the brain is fully developed, which is approximately age 25.”
- “Smoking burnt cannabis can be harmful to the lungs and respiratory system. Choose other methods such as vaporizers but be aware that they still come with risks.”
- “Avoid frequent (daily or near-daily) use.”
- “Avoid deep inhalation or holding your breath after inhaling.”
- “Avoid using large amounts, or cannabis with high potency THC (> 10% THC).”
- “Avoid synthetic cannabinoids.”
- “Ensure your cannabis products are safely stored to avoid accidental ingestion by pets or children.”
- “Consider tracking or monitoring your use to understand your use pattern and when it may be affecting your daily life, or become hard to control.”
- “Only use cannabis products purchased legally to ensure they are free from pesticides and contaminants.”
Managing side effects of cannabis use
Patient follow-up and continued use
As with other non-medical substances, keep apprised of your patients’ use and related concerns. Consider following up more frequently with higher risk populations, including youth and patients with concurrent psychiatric or substance use disorders.
If problematic use or Cannabis Use Disorder is a concern, consider screening your patient using the CUDIT or CAGE for adults or the Brief Screener for Alcohol, Tobacco, and other Drugs for youth.
Patients may also experience additional side effects as a result of cannabis use:
Select side effect to view recommended treatment
Cannabinoid Hyperemesis Syndrome is a syndrome related to cannabis use that causes intermittent cycles of nausea and vomiting. There is limited evidence on the pathophysiology of Cannabinoid Hyperemersis Syndrome (CHS), however it has been recognized with increasing frequency, particularly for patients who have used cannabis frequently and/or chronically.CHS may present similarly to Cyclical Vomiting Syndrome, with cyclic patterns of severe nausea and vomiting over months. Patients with CHS also generally report symptom relief with hot baths or shower.
Recommended treatment
Current treatment for CHS is abstinence and supportive care for hydration and anti-emesis.
For patients presenting with CHS or cyclical vomiting symptoms, recommend patients stop using cannabis.
Patients who use cannabis may experience worsened or new mental health concerns (e.g. depression, anxiety, panic attacks), particularly with high potency THC (>10% THC) cannabis.
The risk of developing psychosis or schizophrenia may increase when cannabis is used more frequently, especially when daily or near-daily use. Additionally the use of high-potency cannabis product has been linked to an increase risk of psychosis.
Recommended treatment
Ensure mental health concerns are treated through non-cannabinoid medication and supportive care (e.g. CBT).
Advise patients that frequent cannabis use may exacerbate mental health issues.
Patients who use cannabis frequently may experience increased incidences of respiratory or lung issues, including shortness of breath or chronic bronchitis.
Recommended treatment
Recommend patients with pre-existing or chronic respiratory issues abstain from cannabis use or consider alternative formulations.
Limited evidence suggests association between elevated blood pressure and heart rate associated with smoked cannabis. This places patients at increased risk of cardiovascular events, including stroke.
Recommended treatment
Advise patients with cardiovascular risk factors or pre-existing cardiovascular events to abstain from cannabis use or consider alternative formulations.
Supporting materials
- Drug Free Kids Canada – Cannabis Talk Kit
- Kahan M, Srivastava A, Spithoff S, Bromley L. Prescribing smoked cannabis for chronic noncancer pain. Can Fam Physician. 2014 Dec;60(12):1083–90.
- Clearing the Air About Marijuana Use
References
-
[1]
Adamson SJ, Kay-Lambkin FJ, Baker AL, Lewin TJ, Thornton L, Kelly BJ, et al. An improved brief measure of cannabis misuse: the Cannabis Use Disorders Identification Test-Revised (CUDIT-R). Drug Alcohol Depend. 2010 Jul 1;110(1–2):137–43.
-
[2]
Legleye S, Guignard R, Richard J-B, Ludwig K, Pabst A, Beck F. Properties of the Cannabis Abuse Screening Test (CAST) in the general population. Int J Methods Psychiatr Res. 2015 Jun;24(2):170–83.
-
[3]
Brown RL, Rounds LA. Conjoint screening questionnaires for alcohol and other drug abuse: criterion validity in a primary care practice. Wis Med J. 1995;94(3):135–40.
-
[4]
Knight, J.R., Sherritt, L., Shrier, L.A., Harris, S.K. & Chang, G. (2002). Validity of the CRAFFT Substance Abuse Screening Test Among Adolescent Clinic Patients. Archives of Pediatrics & Adolescent Medicine, 156, 607–614.
-
[5]
Fischer B, Russell C, Sabioni P, van den Brink W, Le Foll B, Hall W, et. al. Lower-risk cannabis use guidelines: A comprehensive update of evidence and recommendations. AJPH Policy 2017;107(8):e1-12.
-
[6]
Allan GM, Ramji J, Perry D, Ton J, Beahm NP, Crisp N, et. al. Simplified guideline for prescribing medical cannabinoids in primary care. CFP 2018;64:111-120.
-
[7]
Canadian Nurses Association [Internet]. Harm reduction for non-medical cannabis use [cited 2018 Sept 1].
-
[8]
Hall W, Fischer B. “Chapter 8: Harm reduction policies for cannabis” in Harm reduction: evidence, impacts and challenges, European Monitoring Centre for Drugs and Drug Addition. (2010).
-
[9]
Sorensen CJ, DeSanto K, Borgelt L, Phillips KT, Monte AA. Cannabinoid Hyperemesis Syndrome: Diagnosis, Pathophysiology, and Treatment—a Systematic Review. J Med Toxicol. 2017 Mar;13(1):71–87.
Acknowledgments and legal
This Tool was developed as part of the Knowledge Translation in Primary Care Initiative, led by the Centre for Effective Practice with in collaboration with from the Ontario College of Family Physicians and the Nurse Practitioners’ Association of Ontario. Clinical leadership for the development of the tool was provided by Dr. Jonathan Bertram MD CCFP and was subject to external review by health care providers and other relevant stakeholders. This Tool was funded by the Government of Ontario as part of the Knowledge Translation in Primary Care Initiative.
This Tool was developed for licensed health care professionals in Ontario as a guide only and does not constitute medical or other professional advice. Health care professionals are required to exercise their own clinical judgement in using this Tool. Neither the Centre for Effective Practice (“CEP”), Ontario College of Family Physicians, Nurse Practitioners’ Association of Ontario, Government of Ontario, nor any of their respective agents, appointees, directors, officers, employees, contractors, members or volunteers: (i) are providing medical, diagnostic or treatment services through this Tool; (ii) to the extent permitted by applicable law, accept any responsibility for the use or misuse of this Tool by any individual including, but not limited to, primary care providers or entity, including for any loss, damage or injury (including death) arising from or in connection with the use of this Tool, in whole or in part; or (iii) give or make any representation, warranty or endorsement of any external sources referenced in this Tool (whether specifically named or not) that are owned or operated by their parties, including any information or advice contained therein.
Non-Medical Cannabis Resource is a product of the Centre for Effective Practice. Permission to use, copy, and distribute this material is for all non-commercial and research purposes is granted, provided the above disclaimer, this paragraph and the following paragraphs, and appropriate citations appear in all copies, modifications, and distributions. Use of the Opioid Tapering Template for commercial purposes or any modifications of the Tool are subject to charge and must be negotiated with the Centre for Effective Practice (Email: info@cep.health).
For statistical and bibliographic purposes, please notify the Centre for Effective Practice (info@cep.health) of any use or reprinting of the Tool. Please use the below citation when referencing the Tool: Reprinted with Permission from Centre for Effective Practice. (October 2018). Non-Medical Cannabis Resource: Ontario. Toronto: Centre for Effective Practice.
Developed by:
In collaboration with: