This clinical tool aims to support primary care providers in the prevention of childhood obesity within their practice. It is intended to be used with paediatric patients (2-17 years of age) and their families, irrespective of patient weight. This tool was developed to help guide conversations with patients and their families, as appropriate and over a series of visits, that focus on healthy lifestyle choices and goal-setting. Readiness to change and self-efficacy are key concepts within the conversation.
Preventing Childhood Obesity
Discuss healthy lifestyles and agree on a plan
Weight is not always an accurate reflection of lifestyle and nutrition choices. Discussions about healthy and unhealthy choices need to take place with all patients, regardless of how patients track on percentile curves. This section includes tips to help providers initiate discussions about healthy lifestyle choices. Motivational interviewing techniques are suggested to help build rapport and to manage challenging situations. Addressing all aspects of healthy lifestyle and nutrition choices may not be feasible within one visit. The following section acts a guide that can be used over multiple patient visits.
Assess awareness and attitudes towards towards healthy lifestyle habits
Ask patient
- “Do you mind if we take a few minutes to discuss healthy eating and physical activity?”
If patient is ready to discuss
- Ask open-ended questions about concerns: 2
“Do you have any concerns about your/your child’s weight or growth?” - Work with patients and families to identify a lifestyle or nutrition behaviour change goal to discuss (see table below for sample topics and goals).
“Which one of these habits would you like to work on?”
If patient is unsure/unready to discuss
- Acknowledge lack of readiness:
“It seems as if you’re not sure/not ready to discuss this right now. If you want to discuss this later, we can do so at your next visit?” - Continue to track patient’s growth and follow up at next visit.
Select goal and agree on plan
Select a goal
Assist the patient/patient’s family to choose one or more goals tailored to their needs.
Topic area Discussion points Sample goals
Importance of satiety/fullness
- Importance of regular meals and snacks
- Inclusion of protein with all meals and snacks (e.g., protein fortified cereal)
- Liquid protein sources aren’t as effective as solids for fullness (e.g., milk vs. yogurt or cheese)
- Set number of meals with protein/day
- Set number of snacks with protein/week
Household meals
- Reliance on processed foods
- Ultra-processed food and link with obesity
- Cooking is a life-skill to teach our children
- Benefits of family meals (benefits extend beyond nutrition) 3
- Set number of meals cooked with child’s help/week
- Set number of meals eaten together as a family/week
Reduction of liquid calories
- Aim for solid sources of dairy
- Juice should not be considered a fruit equivalent
- Avoid sweet drinks, such as soft drinks, 100% juice, sweetened milk and sports drinks 4
- Set number of drinks/day
Limit eating out
- Food Dollars ($) – over half is spent outside of the house
- Many (96%) fast food kids’ meals exceed recommended daily limits for calories, salt, etc. 5
- Eating patterns set in childhood carry forward to adulthood
- Set number of meals out days/week
- Set number of bagged lunches days/week
Importance of sleep
- Link to obesity
- Screen time before bed (e.g., TVs in bedrooms)
- Set a regular routine
- Sleep apnea
- Benefits beyond nutrition (e.g., mood, concentration)
- Regular sleep time
- Screens off before bed
Physical activity
- Incorporating activity into daily lives (e.g., take a walk in the neighborhood)
- Limit screen time
- Though important to a healthy lifestyle, physical activity cannot offset poor eating habits
- Set number of walks/week as a family
- Playtime outdoors
Explore readiness to work on the goal
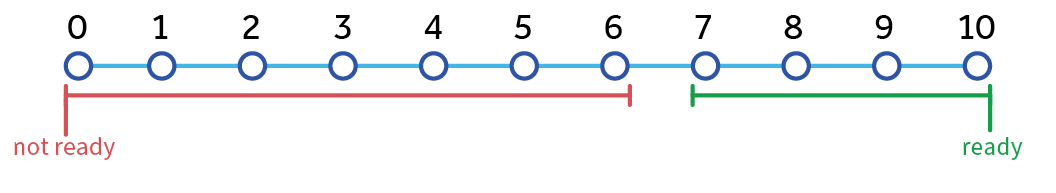
Determine importance
Ask patient: “How important is this change to you?”
Importance Low (< 7) indicates that patient/patient’s family sees healthy lifestyle as unimportant:
- Explore the pros and cons of trying to achieve the ‘agreed-on’ goal vs. the pros and cons of keeping actions the same
- Summarize pros and cons given by patient
- Ask Importance question again:
- If < 7, consider choosing a different goal. If one cannot be found, follow up at next visit.
Determine confidence
Ask patient: “How confident are you about making this change?”
Confidence Low (< 7) indicated patient/patient’s family is unconfident in their ability to change:
- Brainstorm strategies with patient to address potential barriers (e.g., see right) when answering the confidence question
- Adjust goal to be smaller and simpler
- Ask confidence question again
- If < 7, consider choosing a different goal. If one cannot be found, follow up at next visit.
Importance and Confidence High (> 7): Give affirmation of confidence and importance.
Probe to learn more about barriers:
- Food Environment: e.g., cooking skills, kitchen availability
- School: e.g., lunch programs, cafeteria options, bullying
- Socioeconomic status (SES): e.g., single parent, resource constraints for meals (see CEP’s Poverty in Primary Care tool)
- Caregivers: e.g., lack of active play, insufficient nap time7
- Cultural: e.g., traditional diet, beliefs, religion
- Medical Health: e.g., fatigue, chronic conditions, food allergies
- Mental Health: e.g., depression, emotional eating, eating disorders
Managing Challenging Situations
Select situation to view suggestions
- Do not confront or oppose. Instead, make a statement that respects their right to decide and opens the door for future discussion
- Name the emotion, empathize with the patient/family, and explore solutions:
- Do not state facts that counter shared beliefs. Instead, make a statement that reflects what is being said and gives the patient/family an opportunity to voice concerns

If patient is ready for change but family is not:
- Review goal list and help patient choose goals that he/she can do with minimal lifestyle changes from the rest of the family (e.g., consider packing healthier lunch options)
- Work separately with parents to explore their ambivalence toward change.
If family is ready for change but patient is not:
- Probe to learn more about possible barriers to change (see box above) with patient.
- Emphasize adding healthy foods and fun activities with family or friends rather than taking away foods or screen time so plan does not seem punitive.
Agree on a Plan
- Summarize the main points of the discussion and the goal agreed upon.
- Compliment the patient/patient’s family on their willingness to work on healthy living.
- Acknowledge choice and offer encouragement.
- Discuss next steps and follow up at next visit (revisit goals and possibly discuss working on other goals).
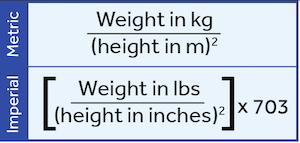
Measure, document, and interpret growth
Measure and document growth
Routine growth monitoring allows providers to identify concerns appropriately, while providing an avenue to prompt healthy lifestyle discussions with patients and families.
- Use quality equipment that is accurate and regularly calibrated to measure patients’ height and weight at both routine and acute/emergent visits.
- BMI is a strong predictor of future risk of becoming overweight and BMI is associated with negative health outcomes. 9, 10
- As childhood BMI is consistent with adult BMI: It can be used to track body size from age 2 through adulthood
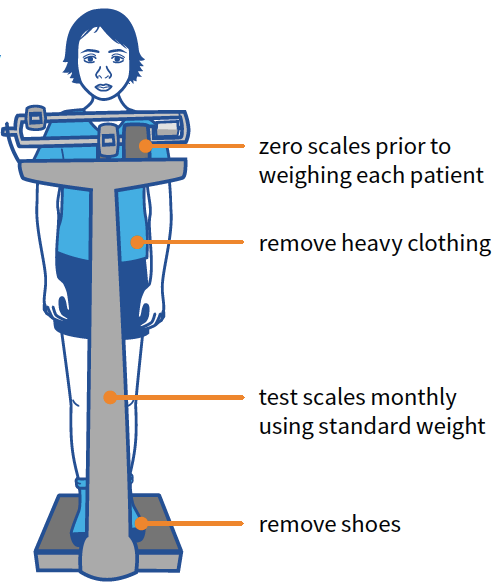
Measuring weight
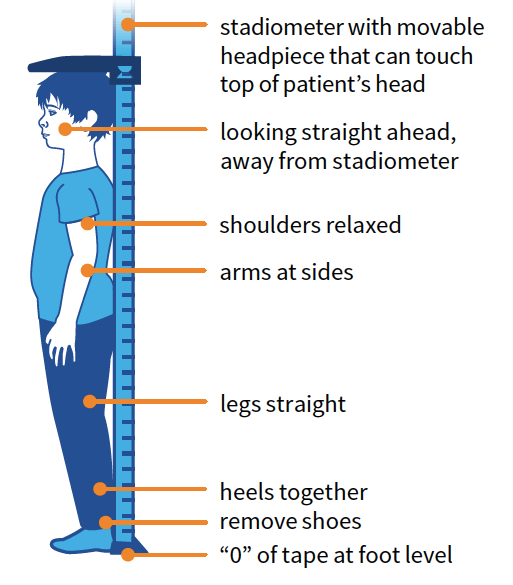
Measuring height
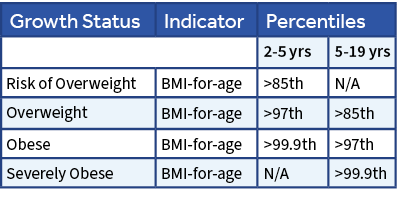
Interpret Growth Data
- The 2014 WHO Growth Charts for Canada represent how typical children should grow over a specific period of time. 11
- For children >2 years of age, the following growth charts are available: 13, 14Weight-for-Age and Length-for-Age
- Body Mass Index (BMI-for-Age)
- WHO recommends BMI-for-Age as the best measure after age 10 due to variable age of puberty – tracking weight alone is not advised. 15
- Percentile curves can be used to understand how the child’s measurements compare to other children of similar age and gender.
- Single measurements may be used to screen for nutritional risk, but have limited use in determining growth patterns and should not be used as diagnostic criteria.
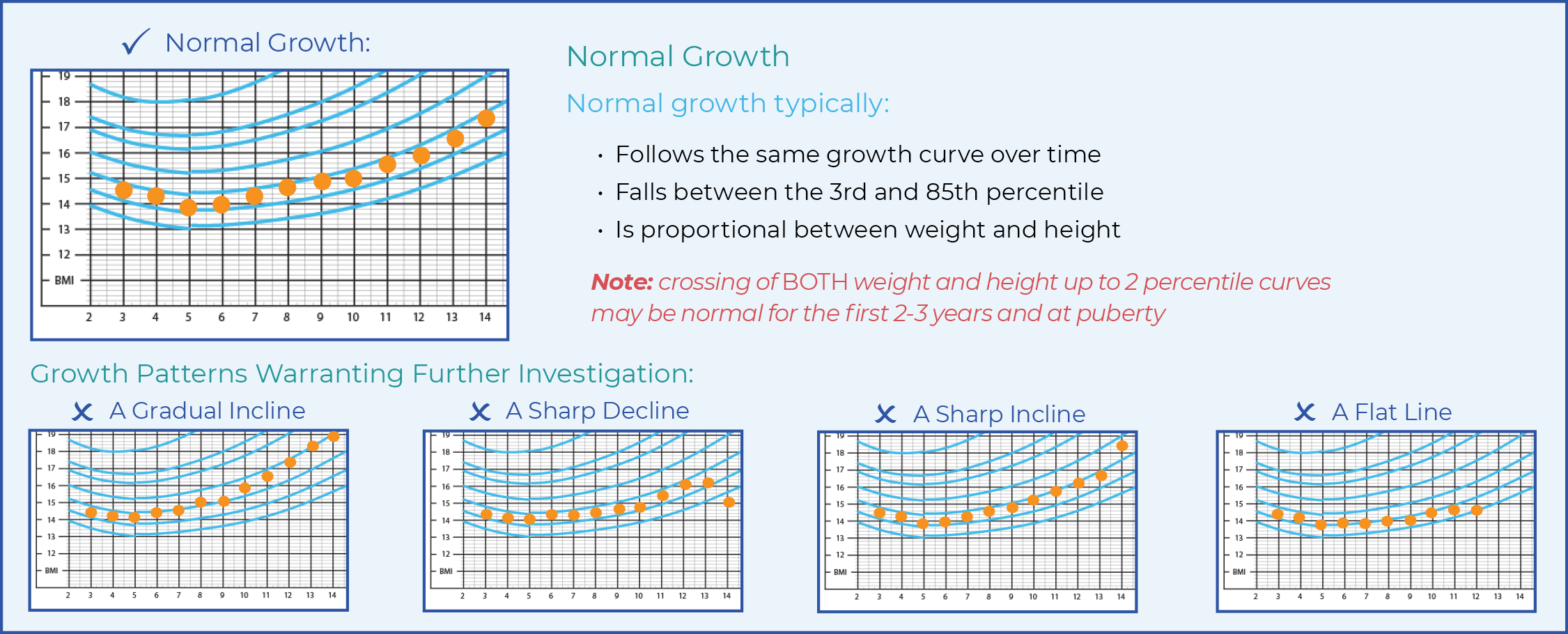
- Plotting and tracking serial weight and length measurements can help to identify children with growth patterns that may warrant further investigation.
Complete healthy lifestyle record
It is important that both providers and patients/families monitor progress towards all ‘agreed-on’ healthy lifestyle goals. Use the Healthy Lifestyle Record to document the patient’s visit, and to summarize the ‘agreed-on’ goals and subsequent plan of action. This Record can be filed in the patient’s chart and referred to during follow-up visits to continue discussions about healthy lifestyle choices.
Supporting materials

For providers
- 2014 WHO Growth Charts for Canada. Recommended for use by the Canadian Collaborative Group (Dieticians of Canada, Canadian Pediatric Society, College of Family Physicians of Canada, Community Health Nurses of Canada, and the Canadian Paediatric Endocrine Group)
- WHO Training Course on Child Growth Assessment. World Health Organization. Training Course on Child Growth Assessment
- WHO Growth Chart Training Program. Dieticians of Canada. A training package on using the WHO Growth Charts for Canada
- Canadian Obesity Network. Clinical tools and resources for managing obesity in primary care
- Change Talk. An online training simulation to practice motivational interviewing techniques for childhood obesity
- Healthy Jacksonville Childhood Obesity Prevention Coalition. Childhood obesity starter kit for the primary care office
- Portico Network. MI resources and training
- Readiness Ruler. A helpful tool to support the use of Motivational Interviewing (MI) by service providers
- Good and Cheap Cookbook. A free cookbook for those on a budget
- EatRight Ontario. Resources and information on children’s nutrition
- Information on Eating Disorders for Medical Professionals
*These supporting materials are hosted by external organizations, and as such the accuracy and accessibility of their links are not guaranteed. CEP will make every effort to keep these links up to date.
References
- [1]
Healthy Jacksonville Childhood Obesity Prevention Coalition. Motivational interviewing: tips for successful physician-patient-family interactions. [cited 2015 Dec 18].
- [2]
Jackson County Weight Collaborative. Childhood obesity provider toolkit. [cited 2015 Dec 18].
- [3]
The Family Dinner Project. Benefits of family dinners. [cited 2015 Dec 18].
- [4]
Campbell M, Benton JM, Werk LN. 5-2-1-Almost None: parents’ perceptions of changing health-related behaviors in their obese child. Perm J. 2009 Summer: 13(3):4-8.
- [5]
Centre for Science in the Public Interest. Kids’ meals II: obesity and poor nutrition on the menu. USA: Centre for Science in the Public Interest; 2013 Mar [cited 2015 Dec 18].
- [6]
Resnicow K, Davis R, Rollnick S. Motivational interviewing for pediatric obesity: conceptual issues and evidence review. J Am Diet Assoc, 2006;106:2024-2033.
- [7]
Martin-Biggers J, Spaccarotella K, Delaney C, Koenings M, Alleman G, Hongu N et al. Development of the intervention materials for the HomeStyles obesity prevention program for parentsof preschoolers. Nutrients. 2015; 7:6628-69.
- [8]
Lorenzetti RC, Jacques CHM, Donovan C, Cottrell S, Buck J). Managing difficult encounters: understanding physician, patient, and situational factors. Am Fam Physician. 2013;87(6):419-25.Tirosh A, Shai I, Afek A, et al. Adolescent BMI trajectory and risk of diabetes versus coronary disease. N Engl J Med 2011; 364: 1315–25.
- [9]
Tirosh A, Shai I, Afek A, Dubnov-Raz G, Ayalon N, Gordon B et al. Adolescent BMI trajectory and risk of diabetes versus coronary disease. N Engl J Med. 2011; 364: 1315–25.
- [10]
Raitakari OT, Juonala M, Viikari JS. Obesity in childhood and vascular changes in adulthood: insights into the Cardiovascular Risk In Young Finns Study. Int J Obes. 2005;29 (Suppl 2): S101–4.
- [11]
Dietitians of Canada and Canadian Paediatric Society. Promoting optimal monitoring of child growth In Canada using the new WHO growth charts: collaborative public policy statement.2010 [cited 2015 Dec 18].
- [12]
2014 Collaborative Group (Canadian Paediatric Society, Canadian Pediatric Endocrine Group, College of Family Physicians of Canada, Community Health Nurses of Canada and Dietitians ofCanada). WHO growth charts adapted for Canada: summary of changes – March 2014. 2014 [cited 2016 Jan 15].
- [13]
Perrin EM, Flower KB, Ammerman AS. Body mass index charts: useful yet underused. J Pediatr. 2004;144(4):455-60.
- [14]
Flower KB, Perrin EM, Viadro CI, Ammerman AS. Using body mass index to identify overweight children: Barriers and facilitators in primary care.Ambul Pediatr . 2007;7(1):38-44.
- [15]
de Onis M, Onyango A, Borghi E, Siyam A, Nishida C, Siekmann J. Development of a WHO growth reference for school – aged children and adolescents. Bulletin of the World HealthOrganization 2007 [cited 2015 Dec 18];85:660-7.
Acknowledgment and legal
This Tool was developed as part of the Knowledge Translation in Primary Care Initiative which is led by CEP with collaboration from OCFP and NPAO. Clinical leadership for the development of the tool was provided by Dr. Yoni Freedhoff MD, CCFP and was subject to external review by primary care providers and other relevant stakeholders. This Tool was funded by the Government of Ontario as part of the Knowledge Translation in Primary Care Initiative.
This Tool was developed for licensed health care professionals in Ontario as a guide only and does not constitute medical or other professional advice. Primary care providers and other health care professionals are required to exercise their own clinical judgment in using this Tool. Neither the Centre for Effective Practice (“CEP”), Ontario College of Family Physicians, Nurse Practitioners’ Association of Ontario, Government of Ontario, nor any of their respective agents, appointees, directors, employees, contractors, members or volunteers: (i) are providing medical, diagnostic or treatment services through this Tool; (ii) to the extent permitted by applicable law, accept any responsibility for the use or misuse of this Tool by an individual including, but not limited to, primary care providers or entity, including for any loss, damage or injury (including death) arising for or in connection with the use of this Tool, in whole or in part; or (iii) give or make any representation, warranty or endorsement of any external sources referenced in this Tool (whether specifically named or not) that are owned or operated by third parties, including any information or advice contained therein.
Preventing Childhood Obesity is a product of the Centre for Effective Practice. Permission to use, copy, and distribute this material for all non-commercial and research purposes is granted, provided the above disclaimer, this paragraph and the following paragraphs, and appropriate citations appear on all copies, modifications, and distributions. Use of Preventing Childhood Obesity tool for commercial purposes or any modification of the tool are subject to charge and use must be negotiated with Centre for Effective Practice (Email: info@cep.health).
For statistical and bibliographic purposes, please notify the Centre for Effective Practice (info@cep.health) of any use or reprinting of the tool. Please use the below citation when referencing the Tool: Reprinted with Permission from Centre for Effective Practice (January 2016). Preventing Childhood Obesity. Toronto: Centre for Effective Practice.
Developed by
In collaboration with