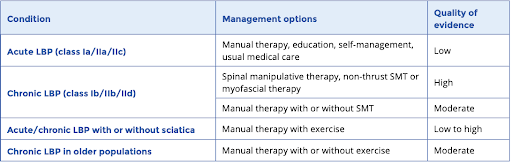
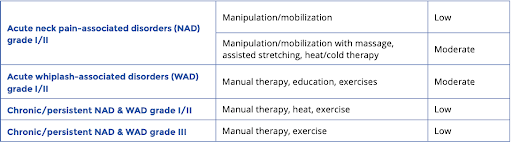
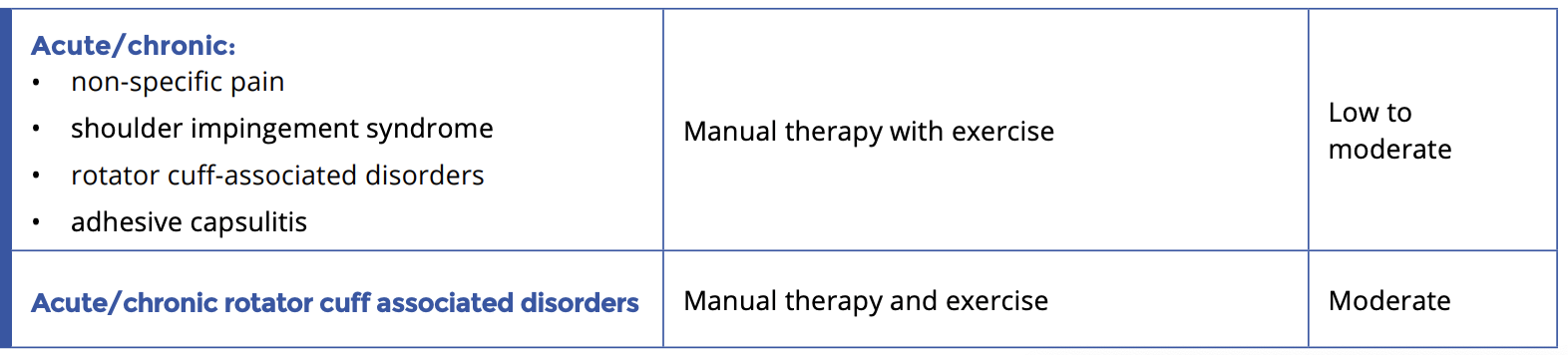
Musculoskeletal (MSK) pain conditions are the biggest cause of disability internationally and a major societal burden.1 However, there is little guidance to assist primary care providers in implementing non-pharmacological treatments such as manual therapy in addition to, or as an alternative for, pharmacological treatment. This tool is designed to increase primary care provider confidence in implementing an evidence-based multimodal program of patient education, exercise and manual therapy for MSK pain.1–10 It will guide providers in the referral for manual therapy by a chiropractor, physiotherapist or registered massage therapist (RMT), and the evaluation of patient outcomes.
Talking Tips
When discussing non-pharmacological treatment options with patients, use motivational interviewing techniques, as appropriate. If patients are reluctant to try something new, try the Elicit-Provide-Elicit technique:
Elicit the patient’s thoughts/feelings:
“How do you feel about trying some exercise or manual therapies for your pain?”
Provide information (a common patient concern is that these therapies will increase pain):
“If I understand correctly, you are concerned that these therapies will increase your pain. However, they can actually help decrease pain over time.”
Elicit the patient’s opinion:
“What do you think about this?”